
Image from https://www.labradorlifeline.org
Arthritis (osteoarthritis – OA) is an inflammatory process effecting one or more joints.
Arthritis can follow any “insult” to a joint – which could be trauma, wear and tear, infection or an inappropriate immune system response. It can happen in any joint, but the larger joints (shoulders, elbows, hips, knees) are more commonly affected.
Younger dogs may become arthritic due to developmental problems which leave the joints poorly formed or formed at an unnatural angle. This can mean the forces going through are not as the joint evolved for, placing the structures under abnormal stress. These problems are often genetic or breed associated. In the majority of cases, there is no obvious root cause, and it is not under an owner’s control.
Arthritis is the most common cause of chronic pain in dogs, it affects 4 out of 5 older dogs. It is often a debilitating, incurable, and progressive disease which initially focuses on moving joints but eventually affects the whole body and is a major cause of euthanasia due to loss of quality of life.
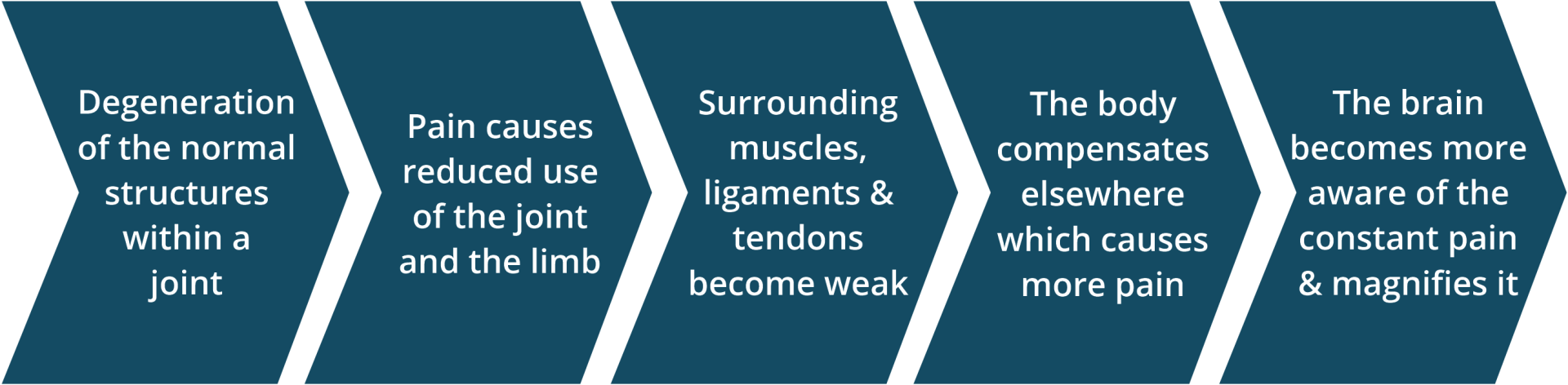
Figure 1
It is a complex disease that requires a dedicated owner collaborating well with their vet to control the disease and maximise quality of life for the dog.
Signs and Diagnosis.
Each dog will present with different clinical signs. Some of these are suggested below. You may notice changes in gait, posture, mobility or behaviour. These can be quite slow to develop, and may be quite vague. There will be ‘good days and bad days’ as the disease progresses. Dogs will usually not show overt pain – they are very good at dealing with it quietly. For example, because they have 4 limbs, they can shift weight, change posture and cope well in the initial stages.
Osteoarthritis tends to reveal itself late in its course. It is common that owners will not notice changes in their dog’s willingness to exercise, ability to do what they used to do, and changes in the way their dog walks and runs, till they have significant arthritis.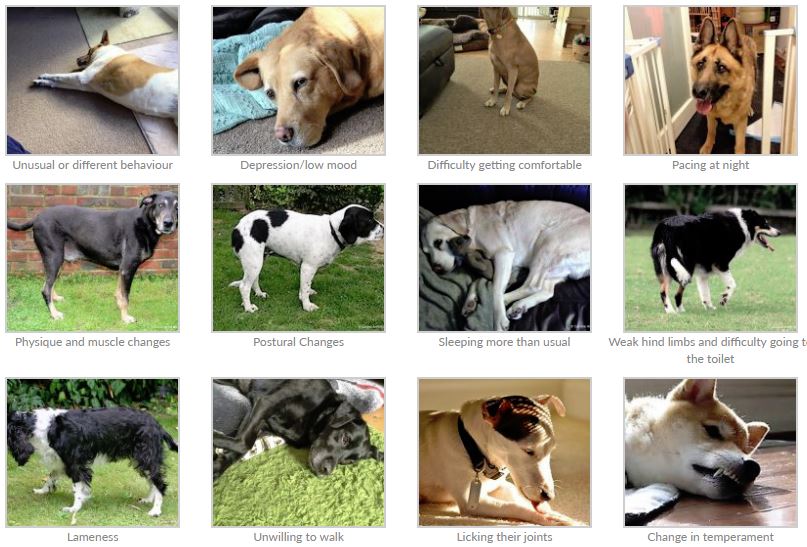
Clinical signs – Figure 2
Your Vet will be able to assess joints for signs of deterioration via a full physical exam. Vets may also recommend X-rays to check for the physical changes of arthritis. Other tests may be necessary to rule out other problems, because the signs can be so non-specific.
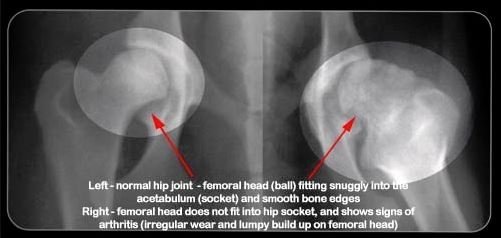
Radiograph showing a normal and an abnormal hip
Arthritis can look very like a number of other diseases, so if further tests are recommended, it will be to rule in or out these other diseases. There are different ways to diagnose arthritis but all are reliant on the owner, noticing that your dog ‘is not right’, is ‘slowing down’, or is ‘getting old’. If you suspect arthritis your dog should have a thorough examination by your vet. There are other conditions that look very similar but require different treatments.
Please speak to a Vet or Nurse early on if you are worried.
Arthritis Management.
Arthritis cannot be cured but it can be well managed. There are many approaches to this and each dog will need a unique plan. Generally, using as many different therapies together is likely to produce the best outcome. It is generally recommended to start with simple changes and work up through the pyramid below as is required by your dog.
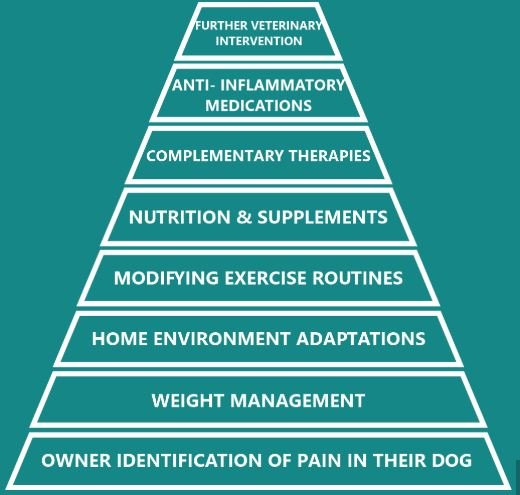
Figure 3
As arthritis progresses, the dog’s ability to cope will deteriorate, limbs weaken and the pain increases. Eventually owners witness their dog not willing to stand up, not willing to walk and not able to interact. At this point, they have lost good quality of life and this is a common reason for euthanasia. This process may be a gradual deterioration or it can happen suddenly.
By intervening, with therapies like in the pyramid above, this process is slowed down, the pain is eased, and mobility, quality of life and the dog – owner bond is maintained. Early identification and action is key to successful osteoarthritis management.
‘Conservative’ Management of the Disease.
Weight management is key and probably the most important single thing we can do early in the treatment plan. This reduces the force going through the unhappy joints every day. Please get in touch with our Nurses who are specially trained to provide weight management clinics for your dog. These are extremely valuable and free of charge.
According to the Kennel Club, 30-60% of adult dogs in the UK are classed as obese. Rather than exact weight, the best way to monitor your dog’s correct size is through “Body Condition Scoring.” You can find lots of examples of these charts online, with either 1-5 or 1-9 scales. This system is based on body shape and what you can feel, and there are often useful pictures attached as a guide.
This alone will make a significant improvement, especially in very overweight dogs.

Body Condition Score – figure 5
Diet is important to control weight and to help general health. Make sure everyone in the household is engaged and on board with the dog’s diet. Look at what you feed, how much you feed, how you feed, how often you feed and when you feed. By considering adjusting other elements of feeding you will have more management options. A good quality diet appropriate to the dog’s weight is recommended. Some diets are specially formulated for overweight and/or older dogs with arthritis. Diets can be best discussed with a Nurse at their clinics. It takes about 4-6 weeks to give a diet a fair trial, so ensure you aren’t changing too often.
Exercise needs to be controlled – light regular work is good, and heavy extended work may do more damage. Ensure you ‘quit while you’re ahead’ and don’t go too far to tire the dog out. Dogs do not think like us, they live in the present, and if the present is exciting and fuelled with new smells, new dogs and new balls, they are likely to temporarily ‘forget’ their discomfort. Adrenaline rushes will also cover up a lot of pain – judge the dog by their behaviour at home, not out on a walk. They are likely to over-do it and suffer the consequences later. Don’t go on surfaces or terrain that is likely to cause slips, trips or falls – accidents are more likely to happen as arthritis progresses.
House adaptations can be helpful to again avoid slips, trips and falls. Most dogs in the UK live in their owner’s home, and may spend up to 90% of their life in that environment. If there are steps that they repeatedly struggle up and down, floors they repeatedly slip on, or solid cold beds they repeatedly sleep on, their condition will not improve as they will continue to injure themselves. Prevent access to stairs or use ramps where this is unavoidable. Put blankets or rugs down on laminate floors to give more grip. Don’t forget to check the garden too! Use a thicker, purpose designed dog bed if possible.
Nutraceuticals or Supplements are common and there is a lot of choice. Many people find these very beneficial for their dog, although there are not many scientific studies about them. They take about 6-8 weeks of use for full effect, and just as in people, some patients respond better than others. Essential Fatty Acids (eg: Omega 3), Glucosamine and Chondroitin are good examples. Good quality, reputable supplements would be recommended – many cheaper ones do not contain all of what they claim on the box but are very well marketed. Some diets may already contain lots of these ingredients.
Complementary therapies are increasingly recognised as hugely influential on dog health, just as in human medicine. The most recommended are acupuncture, physiotherapy and hydrotherapy, but a range of other options are available. Please ask for advice on these, do your research and ensure the provider you use is reputable, qualified and fully licensed. The levels of regulation of this sector are variable and can be quite poor.
Our Southwell practice now offers acupuncture. Hydrotherapy is also highly recommended – find a local centre on the National Association website (https://www.narch.org.uk/Home/Index).
There are a huge number of products and services out there marketed for arthritis in dogs, so ensure you do your research before investing in any product. It is easy to spend unnecessarily, and not all are as good as they seem. Feel free to discuss with a Vet or Nurse beforehand!
Close monitoring and recording can be very helpful to help you and the Vet/Nurse monitor progress over time. Lots of information sheets are available online which will allow you to record diet, weight, mobility and behaviour, among other statistics. Looking for trends can be very useful for disease control. Examples are available on the CAM website: https://www.caninearthritis.co.uk/
Veterinary Interventions in addition to the above.
The Conservative Management should be employed in all dogs but many cases will need further veterinary intervention in conjunction with this.
Pain-relief medications are commonly prescribed. Generally these will include a Non-Steroidal Anti-Inflammatory as a first line treatment. Other drugs may then be used alongside (or rarely, instead of) these drugs to control pain. Each dog will have a unique requirement, so discuss these drugs and their long-term use with your vet.
Non-steroidal anti-inflammatory drugs act to control pain and inflammation. They are considered the mainstay of drug therapy and will be used unless there is another problem that prevents their safe administration. These drugs must not be given with oral steroids unless under specific veterinary advice.
Other drugs that can be added on top of non-steroidal anti-inflammatory drugs include Paracetamol at very specific doses, Amantadine, Gabapentin and Tramadol. These are all human drugs that have been adapted for use in dogs, and so they are “off-license” – no specific dog version exists. This means that these drugs are used with caution – each dog responds differently and so an individual treatment plan has to be developed for each dog.
Surgery for arthritis is not common but is becoming increasingly available. We may recommend ‘arthrodesis’ to permanently immobilise a painful joint. Total joint replacements are now also available for Hips and Elbows. We do not embark on any of these surgeries lightly and the implications must be fully discussed. Most of these surgeries would require a referral from us to a specialist orthopaedic veterinary surgeon.

Total Hip Replacement – Figure 6
It is also possible to inject anti-inflammatory treatments directly into painful and affected joints. At Minster, we have begun investigating this and training staff in this procedure, and so it is something we will now offer in specific cases. Injections can be anti-inflammatory drugs, or biological components harvested and developed from your own dog. The aim of this therapy is to reduce or eliminate the need for long term, whole body medications, where only one or two joints are badly affected.
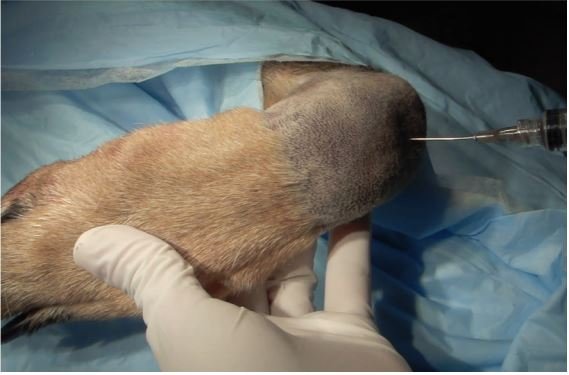
Joint Injection – Figure 7
Further information.
Please discuss any concerns with your vet or nurse at the earliest opportunity. We are happy to help, and discussion is needed to gradually develop a unique plan for every dog.
There are lots of resources available online – do be careful what you read though! The best of these is CAM: Canine Arthritis Management. https://www.caninearthritis.co.uk/
References
This has been heavily inspired by the excellent CAM https://www.caninearthritis.co.uk/
Figures 1, 2 and 4 are from this website.
Figure 3 is from the BVA Website on Hip Dysplasia.
Figure 5 is from the WSAVA Website.
Figure 6 is from Fitzpatrick Referrals regarding Hip Dysplasia.
Figure 7 is from Nupsala (https://www.nupsala.com/wp-content/uploads/2016/08/Companion-Regenerative-U-Guide-to-IA-Injections.pdf).





